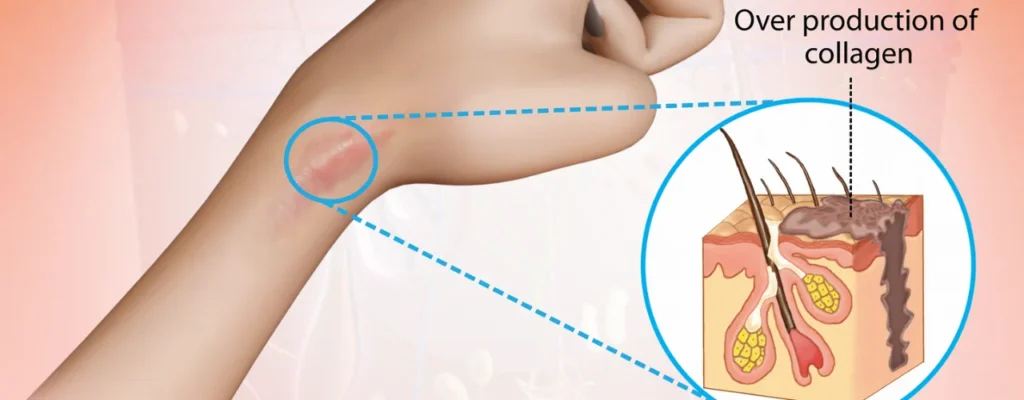
A keloid is a raised scar that grows beyond the original size of a wound. It’s a type of scar tissue that keeps growing abnormally, even after the wound has healed. Keloids can form anywhere on the body, but they’re most common on areas like the chest, shoulders, earlobes, and upper back.
Keloids are more common in people with darker skin tones, particularly those of African, Asian, or Hispanic descent. They can also be more common in people with a family history of keloids.
Causes of keloid:
The exact cause of keloids is unknown, but they’re thought to be caused by an overproduction of collagen, a protein that helps heal wounds. Certain factors can increase your risk of developing keloids, such as:
- Skin injury: Any type of skin injury, such as a piercing, surgery, burn, or acne, can trigger the formation of a keloid.
- Family history: If you have a family history of keloids, you’re more likely to develop them yourself.
- Skin color: People with darker skin tones are more likely to develop keloids.
- Age: Keloids are more common in younger people.
Other factors that may contribute to keloid formation:
- Inflammation: The inflammatory response to a wound may play a role in keloid formation.
- Hormones: Hormonal changes, such as those that occur during pregnancy or puberty, may increase your risk of developing keloids.
- Genetics: Studies have identified several genes that may be associated with keloid formation.
It’s important to note that not everyone who experiences a skin injury will develop a keloid. And, while keloids can be unsightly, they are not cancerous or contagious.
Symptoms of keloids:
Keloids are typically smooth, hairless, and shiny. They can be red, pink, or purple, depending on your skin color. Keloids can also be itchy, tender, or painful.

Appearance:
- Raised and Thick: Keloids are significantly raised above the surrounding skin, giving them a bumpy or lumpy appearance. They can range in size from very small to quite large, even extending beyond the original wound site.
- Smooth and Hairless: Unlike regular scars, keloids are typically smooth and hairless. This is because the excess collagen production disrupts the normal hair growth cycle.
- Shiny Surface: The surface of a keloid is often shiny or reflective due to the dense collagen fibers packed tightly together.
- Color: The color of a keloid can vary depending on your skin tone. It can be red, pink, or purple, and may even darken over time with sun exposure.
Other Symptoms:
- Itching: Keloids can be itchy, especially during the early stages of growth. The itchiness can be mild or quite intense, and may worsen with rubbing or friction.
- Tenderness: Some keloids can be tender or painful, especially when touched or pressed. This is more common in large or rapidly growing keloids.
- Discomfort: The size and location of a keloid can cause discomfort, particularly if it rubs against clothing or restricts movement. This can be a source of both physical and emotional discomfort.
Remember, keloids are not harmful to your health, but they can be a cosmetic concern for some people. If you are concerned about a keloid, it is best to consult with a doctor or dermatologist to discuss treatment options.
Diagnosis of keloid:
Diagnosing a keloid usually involves a combination of the following steps:

Physical examination:
- This is the most important step in diagnosing a keloid. Your doctor or dermatologist will visually examine the affected area, assessing its size, shape, color, texture, and location.
- They will likely inquire about the history of the area, including any recent injuries, piercings, surgeries, or other skin conditions.
Medical history:
- Knowing your family history of keloids can be helpful in the diagnosis, as there’s a genetic component to keloid formation.
- Information about any underlying medical conditions or medications you take can also be relevant, as some can affect wound healing and potentially contribute to keloid formation.
Differential diagnosis:
- Although keloids are distinct, other skin conditions can mimic their appearance, such as hypertrophic scars, dermatofibromas, and keloid mimics (e.g., allergic reactions, pyogenic granulomas).
- Your doctor might need to consider these possibilities and rule them out based on the specific characteristics of the lesion.
Further testing:
- In some cases, particularly when other conditions are suspected, additional tests might be necessary. These can include:
- Skin biopsy: A small sample of tissue is taken from the affected area and examined under a microscope to analyze the collagen structure and differentiate it from other conditions.
- Imaging tests: Rarely, imaging tests like X-rays or ultrasound might be used to assess deeper structures involved in the keloid.
Generally, a physical examination along with a detailed medical history is sufficient to diagnose a keloid. Other tests are mainly used for confirming the diagnosis or ruling out other possibilities.
Treatment of keloid:
Treating keloids can be challenging, as there’s no guaranteed cure and they can recur after treatment. However, several options can help manage their appearance and symptoms:

1. Non-surgical options:
- Corticosteroid injections: Injected directly into the keloid, corticosteroids reduce inflammation and shrink the scar tissue. This is often the first-line treatment, but repeated injections may be necessary.
- Silicone gel sheets: Applying silicone gel sheets over the keloid for several hours daily can help flatten and soften the scar over time. This is a non-invasive and well-tolerated option.
- Cryotherapy: Freezing the keloid with liquid nitrogen can destroy scar tissue and reduce its size. This is effective for smaller keloids and may be combined with other treatments.
- Pressure therapy: Applying pressure garments or silicone pressure sheets can help prevent keloids from growing back after surgical removal.
- Laser therapy: Certain lasers can target and destroy blood vessels supplying the keloid, reducing its size and redness. This option is best for smaller keloids and may require multiple sessions.
- Interferon: Injected interferon alpha can slow keloid growth and reduce inflammation. This is typically used for severe or resistant keloids.
2. Surgical options:
- Surgical excision: Removing the keloid through surgery is an option, but there’s a high risk of recurrence, especially if not combined with other therapies like radiation or pressure therapy.
- Radiation therapy: Low-dose radiation therapy after surgery can reduce the risk of keloid recurrence. However, it may cause side effects like skin discoloration or changes in texture.
3. Other options:
- Topical medications: Corticosteroid creams or ointments can help with itching and inflammation but may not significantly reduce the keloid size.
Choosing the best treatment depends on various factors:
- Size and location of the keloid
- Severity of symptoms
- Previous treatment history
- Individual preferences and medical conditions
It’s crucial to discuss your options with a dermatologist or healthcare professional specializing in keloids. They can recommend the most suitable treatment plan based on your individual needs and assess the potential risks and benefits of each option.
Remember, managing keloids is a process that may require patience and a combination of treatments. Open communication with your healthcare provider is key to achieving the best possible results.
Prevention of keloid:
Preventing keloids entirely is tricky, as the exact cause remains unknown. However, several strategies can significantly reduce your risk, especially if you’re prone to developing them:

Minimize skin injuries:
- Avoid unnecessary procedures: Minimize piercings, tattoos, and elective surgeries, especially in high-risk areas like chest, shoulders, and earlobes.
- Careful wound care: Treat wounds carefully to promote proper healing and minimize inflammation. Keep them clean, moist, and protected from further injury.
- Reduce inflammation: Use gentle methods like cold compresses and over-the-counter pain relievers to manage inflammation after injuries.
Consider preemptive measures:
- Silicone gel sheets: Prophylactically apply silicone gel sheets to areas particularly prone to keloid formation after procedures or injuries.
- Pressure therapy: Use pressure garments or silicone pressure sheets in high-risk areas after procedures or injuries, even if no keloid forms immediately.
Manage known risk factors:
- Family history: If you have a family history of keloids, discuss prevention strategies with your doctor before any procedures or significant skin injuries.
- Skin color: Individuals with darker skin tones are more prone to keloids. Consult a dermatologist familiar with treating keloids in patients with your skin tone for personalized advice.
- Age: Keloids are more common in younger individuals. If you’re considering procedures or have experienced injuries in your youth, prioritize preventative measures.
Remember:
- Early intervention is key: The sooner you implement preventative measures after an injury or procedure, the higher the chance of minimizing keloid formation.
- Consult a dermatologist: If you have a high risk of keloids or concerns about potential formation, seek professional advice from a dermatologist for personalized guidance.
- No guarantees: While these strategies can significantly reduce your risk, they don’t entirely eliminate the chance of keloid development.
Final Conclusion:
Keloids, raised scars prone to excessive growth, while not cancerous, can be bothersome and unsightly. While a cure remains elusive, minimizing skin injuries, practicing diligent wound care, and potentially utilizing preventative measures like silicone gel sheets can significantly reduce their formation. If concerned, consult a dermatologist for personalized advice and treatment options.
Derma and Dental Clinic:
Derma & Dental Clinic stands out with its team of experienced doctors backed by scientific evidence in their chosen fields. Their diverse range of medical-grade procedures offer tailored solutions for various skin and dental needs. You can confidently book your consultation online or by phone and embark on your journey towards healthier skin and a radiant smile.
Location: Bahria Town, Lahore
Specialties: Dermatology and Dental Care
Website: Derma.pk
For Appointment:
- Online at Dermatology.pk
- WhatsApp: +923205999650
- Phone: 03041115000



















[…] Conquer Keloids: Prevent Scar Growth and Restore Confidence […]