Introduction:
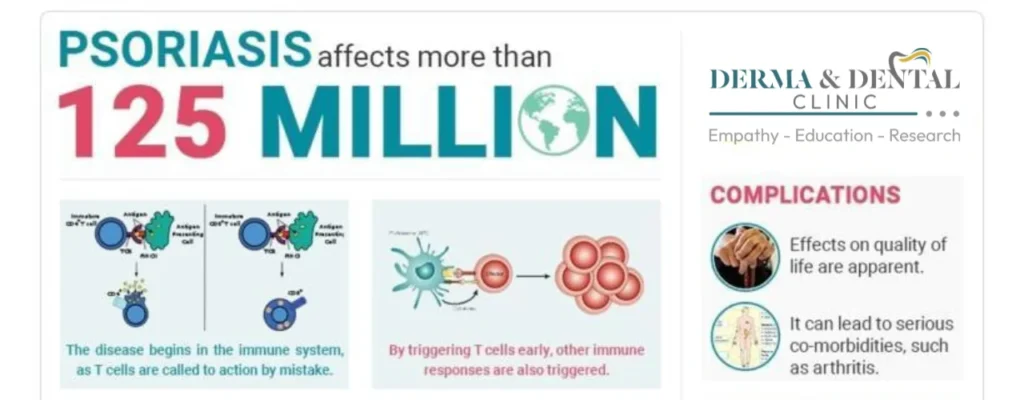
Psoriasis is a chronic, autoimmune skin condition that causes skin cells to grow too quickly, resulting in raised, red, scaly patches. It’s a relatively common condition, affecting about 2% of the population worldwide.
The immune system malfunction:
- Imagine your immune system as a security guard constantly scanning for threats. Normally, it targets harmful invaders like bacteria or viruses.
- In psoriasis, this “guard” misidentifies healthy skin cells as enemies and triggers an inflammatory attack.
- This leads to rapid skin cell growth, exceeding the normal shedding rate. Dead skin cells pile up, forming thick, red, scaly patches.
Impact on the skin:

- These patches, called plaques, are the hallmark symptom. They can appear anywhere on the body, with common locations being elbows, knees, scalp, and lower back.
- The plaques can be itchy, sore, and sometimes painful. They can also crack and bleed, especially with scratching.
- In severe cases, the plaques can cover large areas of the body, causing significant discomfort and even affecting joints (psoriatic arthritis).
Beyond the skin:
- Psoriasis is more than just a skin condition. The inflammation can affect other body systems too.
- People with psoriasis have a higher risk of developing certain health problems like heart disease, depression, and anxiety.
- Early diagnosis and effective management are crucial to minimize these risks and improve overall well-being.
Causes of Psoriasis:
While the exact cause remains a mystery, researchers believe it’s a complex interplay of factors:
1. Genetics: Psoriasis has a strong genetic component. Having specific genes increases your susceptibility to the condition, especially if someone in your family has it. However, having the genes doesn’t guarantee developing psoriasis, and not everyone with a family history gets it.
2. Immune System: Psoriasis is considered an autoimmune condition. This means that your immune system, which normally fights off pathogens, mistakenly attacks healthy skin cells. This triggers inflammation and rapid skin cell growth, leading to the characteristic plaques.
3. Environmental Triggers: Certain factors can act as triggers, worsening existing symptoms or even sparking the initial onset:
- Stress: Emotional stress can be a potent trigger for psoriasis flare-ups. Managing stress through techniques like relaxation exercises or therapy can be helpful.
- Skin Injuries: Cuts, scrapes, sunburns, or even insect bites can trigger psoriasis patches to develop at the injured site, known as the Koebner phenomenon.
- Infections: Strep throat and other infections can sometimes trigger psoriasis, particularly guttate psoriasis (small, teardrop-shaped lesions).
- Medications: Certain medications, like lithium, beta-blockers, and anti-malarials, can trigger or worsen psoriasis.
- Weather: Cold, dry weather can exacerbate symptoms, while warm, sunny climates can offer some relief.
- Smoking and Alcohol: Smoking and excessive alcohol consumption are known to worsen psoriasis symptoms.
It’s important to remember:
- Psoriasis is not contagious. You cannot get it from someone else.
- Finding your individual triggers can help you manage your psoriasis better.
- Combining lifestyle changes with appropriate medical treatment can significantly improve your quality of life with psoriasis.
Sign and symptoms of Psoriasis:
Psoriasis’s symptoms can vary widely from person to person, but some common ones include:

Skin:
- Thick, red, scaly patches: These raised lesions, called plaques, are the most common symptom. They can appear anywhere on the body, although elbows, knees, scalp, and lower back are frequent spots.
- Itching, burning, or soreness: The affected skin can feel itchy, burning, or even sore, making it uncomfortable and potentially impacting sleep.
- Dry, cracked skin: The rapid skin cell growth can lead to dryness and cracking, especially in areas like hands and feet.
- Silver-white scales: The dead skin cells pile up, forming silvery-white scales that cover the plaques.
Nail changes:
- Pitting: Tiny dents or holes can appear on the nails, giving them a rough texture.
- Discoloration: The nails may turn yellow, brown, or white.
- Crumbling or separation: In severe cases, the nail may even crumble or detach from the nail bed.
Joint pain and stiffness:
- Psoriatic arthritis, a related condition, can cause joint pain, stiffness, and swelling, particularly in the fingers, toes, knees, and ankles.
Other potential symptoms:
- Fatigue: The inflammation associated with psoriasis can cause general fatigue and tiredness.
- Emotional impact: Living with a chronic skin condition like psoriasis can take a toll on mental health, leading to anxiety, depression, or low self-esteem.
It’s important to note that:
- The severity of symptoms varies greatly. Some people may only have mild patches, while others experience widespread and severe involvement.
- Psoriasis can also go through cycles of flares and remissions, meaning symptoms may worsen for periods and then improve or even disappear for a while.
- If you notice any of these symptoms, it’s crucial to consult a doctor or dermatologist for proper diagnosis and treatment. Early diagnosis and management can help control symptoms and improve quality of life with psoriasis.
Types of Psoriasis:
Psoriasis comes in several forms, each with its own distinct characteristics and presentation. Here’s a breakdown of the most common types:
1. Plaque Psoriasis: The most prevalent form, affecting around 80% of people with psoriasis. It manifests as:

- Raised, red patches (plaques) covered in silvery-white scales.
- Commonly affects elbows, knees, scalp, and lower back, but can appear anywhere.
- Itching, burning, or soreness in the affected areas.
2. Guttate Psoriasis: Often triggered by infections, particularly strep throat, it presents as:

- Small, red, teardrop-shaped lesions, typically on the torso, limbs, and scalp.
- Less common than plaque psoriasis, mostly affecting children and young adults.
- Usually clears up within weeks or months without treatment.
3. Pustular Psoriasis: Characterized by:

- White pustules surrounded by red, inflamed skin.
- Most commonly affects hands and feet, but can also appear on other areas.
- Two main types: localized and generalized, with the latter being more severe and requiring immediate medical attention.
4. Inverse Psoriasis: Develops in:

- Smooth, red patches in skin folds, like under the breasts, in the groin, or armpits.
- Less common than plaque psoriasis.
- Often mistaken for fungal infections.
5. Erythrodermic Psoriasis: A rare and severe form, characterized by:

- Widespread redness, flaking, and burning affecting large areas of the body.
- Can be life-threatening if not treated promptly.
- Requires hospitalization for intensive care.
Beyond these, other less common types exist, like:
- Nail psoriasis: affecting the fingernails and toenails, causing pitting, discoloration, and abnormal growth.
- Psoriatic arthritis: a form of arthritis affecting people with psoriasis, causing joint pain, stiffness, and swelling.
Treatment of Psoriasis:
While there’s no cure for psoriasis, a range of treatment options can help manage symptoms and improve your quality of life. The best approach for you will depend on the severity and type of psoriasis you have, along with your individual preferences and health conditions. Here’s a breakdown of the main categories:
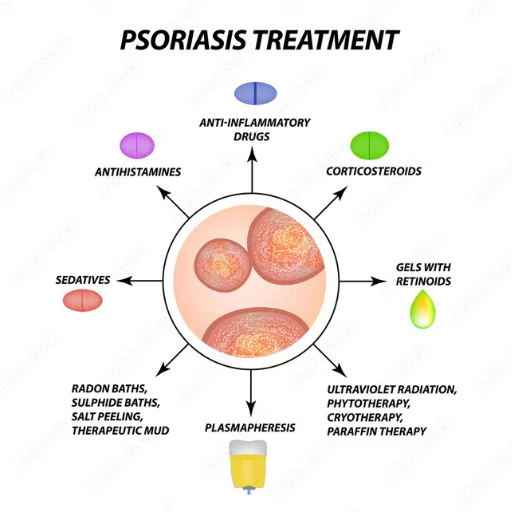
1. Topical Treatments:
- Over-the-counter: Mild to moderate psoriasis often responds well to creams and ointments containing corticosteroids, vitamin D analogs, or salicylic acid.
- Prescription: Stronger corticosteroids, coal tar preparations, and calcineurin inhibitors may be prescribed for more severe cases.
2. Light Therapy:
- Ultraviolet B (UVB) therapy: Exposing the skin to controlled doses of UVB light can slow skin cell growth and reduce inflammation.
- Excimer laser: A targeted form of UVB therapy for small, resistant areas.
3. Systemic Medications:
- Methotrexate: An immunosuppressant medication that slows down skin cell growth.
- Cyclosporine: Another immunosuppressant with similar effects to methotrexate, but with more potential side effects.
- Apremilast: A newer oral medication that targets an inflammatory pathway involved in psoriasis.
- Retinoids: Synthetic forms of vitamin A that can help normalize skin cell growth.
4. Biologic Therapies:
- Targeted injectable or intravenous medications: Highly effective for moderate to severe psoriasis by blocking specific proteins involved in the immune system’s inflammatory response.
- Examples include:
1. Adalimumab
2. Secukinumab
3. Ustekinumab
4. Infliximab
5. Efalizumab
6. Etanercept
7. Certolizumab pegol
5. Other Therapies:
- Phototherapy combined with medication: Combining light therapy with other treatments can enhance efficacy.
- Lifestyle modifications: Managing stress, maintaining a healthy weight, and quitting smoking can improve psoriasis symptoms.
- Psychological support: Psoriasis can affect mental well-being, so seeking therapy or joining support groups can be beneficial.
Remember, choosing the right treatment requires consultation with a dermatologist or healthcare professional. They can assess your individual needs, discuss the risks and benefits of each option, and develop a personalized treatment plan.
Here are some additional points to consider:
- Treatment may need to be adjusted over time as your psoriasis responds or changes.
- Some treatments may have side effects, so it’s important to weigh the risks and benefits with your doctor.
- Don’t be discouraged if a treatment doesn’t work immediately. Different approaches may be needed to find the best fit for you.
https://blog.derma.pk/?s=narrow+band
Final Thoughts:
Psoriasis, while an incurable skin condition, is far from uncontrollable. Understanding its causes, symptoms, and various treatment options empowers you to manage it effectively and live a fulfilling life. Remember, with early diagnosis, comprehensive treatment, and a proactive approach, you can significantly minimize psoriasis’s impact and maintain vibrant well-being.
Derma and Dental clinic:
Derma & Dental Clinic stands out with its team of experienced doctors backed by scientific evidence in their chosen fields. Their diverse range of medical-grade procedures offer tailored solutions for various skin and dental needs. You can confidently book your consultation online or by phone and embark on your journey towards healthier skin and a radiant smile.
Location: Bahria Town, Lahore
Specialties: Dermatology and Dental Care
Website: Derma.pk
For Consultation:
- Online at Dermatology.pk
- WhatsApp: +923205999650
- Phone: 03041115000



















Hi there, I found your website via Google while searching for a related topic, your website came up, it looks great. I have bookmarked it in my google bookmarks.
I’m truly enjoying the design and layout of your site. It’s a very easy on the eyes which makes it much more enjoyable for me to come here and visit more often. Did you hire out a developer to create your theme? Outstanding work!